Daily incidence map
(14-Day Mov. Average)
Notes: Moving averages are 7-day backward. The number is based on the daily value. It is assumed to be the same as the previous day if not updated. On the days with no continuity from the previous day due to change of standards, "New" number is treated as 0 and the bar color is changed. Data may be corrected by the developer when it is considered as an obvious misstatement, such as minus value of Tested Positive.
Resources: EODY. Measures by Covid-19-Response-Greece. Data on prefectures were taken from EODY, covid19.gov.gr. (Special thanks to @Nyrro for the initial data). Data on the vaccinations by age groups were taken from ECDC. Predictions were taken from covid19-projections.com, covid19.healthdata.org. Used introductory text for IIFR from WHO and prediction model from (link1, link2, link3).
Effective Reproduction number RJ algorithm taken from American Journal of Epidemiology and Richard Schubert. Used Chart.js and highcharts to draw the charts.
Original template by: TOYO KEIZAI ONLINE
Frequently Asked Questions
Q. Why do some values reported by EODY don't coincide with the values on the graphs?
A. This usually happens when yesterday's daily report contains errors or some values need to be updated. These changes occur in the next daily report.
Q. Why do some values show a negative value, even though they shouldn't ?
A. It happens when the previous data have been corrected or there are no available data on the next day. When previous numbers contain errors, any corrections to the final values are made in the next daily report. The above does not apply in the cases of "Critically Ill" section. Negative values in this section means a patient has either left the intensive or sadly has died.
Q. What is the definition of "Critically Ill"?
A. It means cases where the patient is provided with respiratory support. (intubation)
Q. How accurate is the Active Cases section?
A. It is only an estimate based on the assumption that most people recover from a mild form of COVID-19 within two (Delta) one week and in the most severe cases within three (Delta) two weeks (average), giving an absolute median of 17 (Delta) 8 days. Subtracting the number of cases that were found positive when entering the country as well as the number of deaths per day from the total number of daily cases we find the average number of active cases per day. To give an example (Delta), the sum of all cases from 17 days before the 7th of August was 1222. We also had 13 deaths and a total of 261 cases related to travel from abroad. Subtracting the above 2 values from the total number of cases we have (approximately) 896 active cases.
It is worth noting that when this graph reaches zero we can not assume that the epidemic has stopped due to the stochastic nature of the data. However, a rise of the graph after a decline can indicate that a second wave is coming.
Q. What is Effective Reproduction Number Rj?
Often, estimation of the effective reproduction number is a complicated affair, because only the epidemic curve is observed and there is no information about who infected whom. Recent analyses of closely monitored epidemics have shown that it is possible to estimate the probability that one person has infected another if the spatial locations of the infected persons are available. However, when only times of symptom onset are available, most investigators resort to approximating 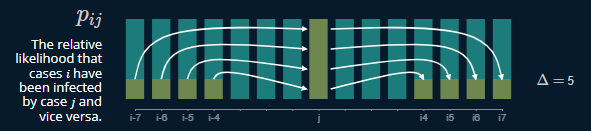 The estimation algorithm allows estimation of the effective reproduction numbers for infectious diseases at a finer temporal resolution under more general assumptions than was previously possible.
The estimation algorithm allows estimation of the effective reproduction numbers for infectious diseases at a finer temporal resolution under more general assumptions than was previously possible.
Q. How is the «True» number of infections been produced?
Knowing the true number of people who are infected with COVID-19 is an essential step towards understanding the disease. But estimating this number is not a simple task. The true number of infections is many times greater than the reported number of cases because the majority of infected individuals do not get tested due to several reasons: 1) they are asymptomatic, 2) they are only mildly symptomatic, 3) they do not have easy access to testing, or 4) they simply do not want to.
The core idea behind this method is that we can use the positivity rate to roughly determine the ratio of true infections to reported cases. The hypothesis is that as positivity rate increases, the higher the true prevalence in a region relative to the reported cases. This also makes sense intuitively: if you test everyone, then the positvity rate will be very low, and you will catch every case. But if testing is not widely available, then you will catch only the severe cases, resulting in a higher positivity rate. This phenomenon is sometimes referred to as preferential testing. The exact relationship varies from region to region and across time. But if one were to take the average across all of the data, one can generate a theoretical curve. This relationship can be approximated by a root function of the following form: prevalenceRatio = a * (positivityRate)^(b) + c, where
Q. What is the positivity rate?
A. The positive rate is just the fraction of the tests that come back positive. It is calculated by dividing the number of positive confirmed cases by the total number of tests performed. A 7-day moving average is used in all of our calculations, so the same applies here.
Q. What is the Implied Infection Fatality Rate (IIFR)?
A. An important characteristic of an infectious disease, particularly one caused by a novel pathogen like SARS-CoV-2, is its severity, the ultimate measure of which is its ability to cause death. Fatality rates help us understand the severity of a disease, identify at-risk populations, and evaluate quality of healthcare. There are two measures used to assess the proportion of infected individuals with fatal outcomes. The first is infection fatality ratio (IFR), which estimates this proportion of deaths among all infected individuals. The second is case fatality ratio (CFR), which estimates this proportion of deaths among identified confirmed cases. To measure IFR accurately, a complete picture of the number of infections and deaths caused by the diseasem must be known. Consequently, at this early stage of the pandemic, most estimates of fatality ratios have been based on cases detected through surveillance and calculated using crude methods, giving rise to widely variable estimates of CFR by country – from less than 0.1% to over 25%. For COVID-19, as for many infectious diseases, the true level of transmission is frequently underestimated because a substantial proportion of people with the infection are undetected either because they are asymptomatic or have only mild symptoms and thus typically fail to present at healthcare facilities. Since a complete picture of the number of infections and deaths is not yet possible, as the pandemic is still ongoing, we can express all of the above in an equation using the values of the "true" number of infections and reported deaths. Although this is by no means a complete equation, at least in this way we approach (within a reasonable framework) a value that helps us to better understand the changing dynamics of this disease and its impact on the population.
The IIFR is a metric derived by taking the reported deaths and dividing them by the true infections estimate (after accounting for lag, 28 days delay). Note that we assume that the reported deaths are approximately equal to the actual deaths. If there is a significant number of exaggerated / unreported COVID-19 deaths, then the IIFR estimate will be lower than the actual IFR. For all values, a 7-day average was used.
- Lower median age of infection
- Better protection of vulnerable populations
- Improved treatment (new drugs, better allocation of resources, more experience among staff, etc)
- Earlier detection
The above are explanations that would explain a true decrease in IFR. A lower median age of infection and better protection of high-risk populations are probably the primary drivers behind the decrease in IIFR. Below are some reasons that could skew the IIFR lower, but not change the true IFR:
- More comprehensive reporting of confirmed cases
- Changes in the distribution of age groups tested (e.g. more younger people getting tested would skew IIFR down)
- Inflation of the test positivity rate (e.g. double-counting positives, not reporting negatives, etc)
- Longer lag in death reporting
- Underreporting of deaths
Q. Can I use the data?
A. Yes, feel free to use it for both commercial or non-commercial use. If you'd like just mention my name Sandbird. Other specific standards are based on the MIT license and our Privacy Policy.